
What is a heart attack?
The most common cause of a heart attack is coronary heart disease.
Key takeaways
2 min read
Always call Triple Zero (000) immediately if you think you or someone else may be having a heart attack.
A heart attack occurs when a coronary artery, which supplies blood to your heart, becomes blocked.
The most common sign of a heart attack is chest discomfort or pain, which can spread to your arms, neck, jaw or back.
Chest discomfort or pain can last for several minutes or come and go.
A heart attack requires emergency treatment to restore blood flow to your heart.
The heart is a muscular pump that’s a little larger than your fist. It’s one of your most important muscles as it pumps blood all over your body through the circulatory system.
Your blood carries oxygen, which is needed by every cell in your body, all the time. Your heart pumps oxygen-rich blood from the lungs to the heart, and then on to the rest of the body.
What is a heart attack?
For your heart to function properly, it needs a good blood supply. A heart attack occurs when a coronary artery, which supplies blood to your heart, becomes blocked. This stops the blood flow and reduces the amount of oxygen that gets to your heart muscle. This causes the most common heart attack symptoms, which are chest discomfort or pain and can spread to your arms, neck, jaw or back. Unlike angina this discomfort often last for longer than 10 minutes.
Your heart can be damaged by interrupted blood flow caused by a heart attack. The longer the blockage is left untreated the more the damage occurs. Without urgent treatment to restore the blood flow, the damage can be permanent.
A heart attack can be fatal. Each day, an average of 19 Australians die from a heart attack. One patient is admitted to an Australian hospital with a heart attack every nine minutes.
If you, or someone you know, is experiencing heart attack symptoms for greater than 10 minutes of rest, or if symptoms are severe, or they are getting worse, call Triple Zero (000) immediately.
A heart attack can also be called a myocardial infarction (MI).
What causes a heart attack?
The most common cause of a heart attack is coronary heart disease. This occurs when the coronary artery, which supplies blood to your heart, narrows because of a build-up of plaque. Plaque is made of fat, cholesterol and other materials. The narrowed artery causes a reduced amount of blood flow to your heart muscle.
During a heart attack, plaque from the artery wall breaks away (ruptures) and can form a clot. This can block the flow of blood through the artery and cause damage to the heart muscle.
Do you know your risk of heart attack or stroke? Ask your GP if you are eligible for a Heart Health Check. What is a Heart Health Check?
Other causes of heart attack besides blockage
Not all heart attacks are caused by coronary heart disease and plaque rupture.
Some heart attacks are caused when a coronary artery contracts (spasms) and narrows. Like coronary heart disease, this also reduces or stops blood flow reaching your heart. If an artery has a severe spasm, it can cause a heart attack.
A heart attack can also be caused by the tearing of the coronary artery wall (spontaneous coronary artery dissection).
What is the difference between heart attack and cardiac arrest?
Heart attack
A heart attack occurs when an artery supplying blood to your heart becomes blocked, which stops blood flow and reduces the amount of oxygen that gets to your heart.
A person having a heart attack is usually conscious and may be complaining of chest discomfort or pain or other symptoms.
Cardiac arrest
A cardiac arrest occurs when your heart stops beating due to an electrical malfunction.
A person in cardiac arrest will be unconscious (not able to respond) and will not be breathing. This is because their heart has suddenly stopped beating and blood can no longer flow to the brain, heart and lungs.
A cardiac arrest is a medical emergency. If the heart is not restarted immediately, cardiac arrest can lead to brain damage and then death. Every second counts. If you witness a cardiac arrest call Triple Zero (000) immediately. Giving chest compressions and using a defibrillator (AED) can improve a person’s chances of survival.
Heart attack warning signs and symptoms
Recognising the symptoms of a heart attack and calling Triple Zero (000) could save your life or the life of a loved one. It’s important that people of all genders know the warning signs and symptoms of a heart attack, because early treatment is vital. The longer a blockage is left untreated, the more damage occurs.
The most common heart attack warning signs are:
Chest discomfort or pain (angina). This can feel like uncomfortable pressure, aching, numbness, squeezing, fullness or pain in your chest. This discomfort can spread to your arms, neck, jaw or back. It can last for several minutes or come and go
Dizziness, light-headedness, feeling faint or feeling anxious
Nausea, indigestion, vomiting
Shortness of breath or difficulty breathing – with or without chest discomfort
Sweating or a cold sweat.
How do you know if you’re having a heart attack and not something less serious?
Heart attack symptoms can be different for each person. No two heart attacks are the same, even for the same person. You may have just one, or a combination of symptoms. Sometimes the symptoms of a heart attack are not the classic ‘crushing chest pain’ you may expect.
You may feel less obvious symptoms, such as a burning feeling in your chest and shortness of breath. Sometimes you may have no ‘warning sign symptoms’ at all. In fact, your doctor may even discover that you have had a silent heart attack.
A heart attack can only be diagnosed by medical tests. The only way to know what you’re experiencing is to seek urgent help. At worst, you may have something less serious. At best, you will receive the treatment that you need.
Do not ignore the warning signs of a heart attack. Every minute counts.
Access free heart attack warning signs education, action plans and videos.
If you’re experiencing the warning signs of a heart attack or are worried you or someone you know is having a heart attack – tell someone. If symptoms are severe, or getting worse, or last for more than 10 minutes, call Triple Zero (000) immediately.
How can you reduce your risk of having a heart attack?
Knowing your risk of coronary heart disease is the first step to reducing your risk of having a heart attack. Yet many people don’t know that they are at risk. Almost all Australians (99%) have at least one risk factor for heart disease, and more than half (57%) have three or more risk factors.3
The best way to find out your risk of having a heart attack is to see your GP for a heart health check if you are over the age of 45 (or 30 for Aboriginal and Torres Strait Islander people).
You can reduce your risk by making positive changes to your lifestyle with the help of your doctor.
How is a heart attack diagnosed?
A heart attack is a medical emergency. If you’re experiencing the symptoms of a heart attack, call Triple Zero (000) and ask for an ambulance. An ambulance is the safest way to go to hospital and the quickest way to seek treatment. Treatment can start when ambulance staff arrive, saving precious minutes and preventing damage to your heart muscle.
Once you get to hospital, your doctor will perform tests to diagnose if you’re having a heart attack.
These tests will also measure the amount of damage caused to your heart and the best treatment course to take.
These tests include:
Electrocardiogram (ECG)
Blood tests
Coronary catheterisation (angiogram)
How is a heart attack treated?
A heart attack requires emergency treatment to restore blood flow to your heart. The faster this happens, the less the heart muscle is damaged. Heart attack treatments may involve medications or surgery.
Medications for a heart attack
Your doctor may prescribe several medications to treat your heart attack. It’s very important to never stop taking your medication unless your doctor or cardiologist tell you to do so.
Anticogulant medicines
These are also known as “blood thinners”. They reduce your blood’s clotting action to prevent clots from forming and stop existing clots from growing bigger. In a heart attack, anticoagulant medications may be given to you in a drip, an injection in the stomach or as tablets. Depending on which anticoagulant you’re prescribed, regular blood tests may be necessary to monitor your risk of bleeding.
Antiplatelet meicines
These can be used with other drugs to stop new blood clots forming and existing blood clots from getting bigger. You usually need antiplatelet medicines if you’ve had a previous heart attack or angina, especially if you’ve had stent surgery.
Beta - blockers
These medications help relax your heart muscle, slow your heartbeat and lower your blood pressure. This reduces the load on the heart and lowers your risk of a heart attack. You may be prescribed a beta-blocker for arrhythmia (abnormal heart rhythm) or angina.
Blood pressure medications
Angiotensin converting enzyme (ACE) inhibitors widen (‘dilate’) your blood vessels to reduce the strain on your heart. They are used to lower your blood pressure, make your heart work better and improve your chance of surviving after a heart attack. Angiotensin II receptor blockers (ARBs) work like ACE inhibitors. They may be prescribed if you have side effects, such as a persistent cough, from taking ACE inhibitors.
Chest pain relivers (nitrates)
These medications increase blood flow to your heart by widening your blood vessels. They prevent or treat chest pain or angina. These medications can be in a table, patch or spray form.
Statins
These medications reduce your risk of heart attack by helping to lower your cholesterol. If you have had a heart attack, you may be prescribed statins, even if your cholesterol level is within the normal range.
Thrombolytics
These “clot busting” medications dissolve any blood clots that may be narrowing or blocking your arteries. They are given by an injection into a vein.
Surgical procedures for a heart attack
Coronary angioplasty, percutaneous coronary intervention or stents
This procedure uses a tiny balloon to widen your narrowed arteries. It’s often carried out at the same time as a coronary angiogram. A long tube (catheter) with a tiny balloon on the end is put into an artery in your groin, arm or wrist. It’s guided up into the heart’s artery. The balloon is blown up at the narrowed part of your artery. The cardiologist inserts a small mesh tube (stent) to keep the artery open after the catheter is removed.
Coronary artery bypass graft surgery (CABG)
This type of surgery also improves blood flow to the heart. A healthy blood vessel (or more than one) is taken from your chest, leg or arm, and attached (grafted) to each side of your blocked artery. This lets blood go around or ‘bypass’ the blockage.
You will usually stay in hospital for two to five days after a heart attack, depending on what treatment/s you have had and how well you begin to recover.
Life after a heart attack
A heart attack can be a terrifying experience. It’s normal to be worried about your recovery and future. But you’re not alone. Around 150 Australians are admitted to hospital for a heart attack each day.
Many people make a full recovery and return to their normal activities. Cardiac rehabilitation is an excellent way to recover from a heart attack, manage your risk factors and return to live a full and active life.
Having one heart attack increases your risk of having another. It’s good to know that this risk is greatly reduced with the correct treatment and management. After a heart attack, your healthcare team will help you learn how to manage your heart health for life.
Where to get support after a heart attack.
References
1. Australian Bureau of Statistics. Causes of death, Australia. https://www.abs.gov.au/statistics/health/causes-death/causes-death-australia/2022
2. Australian Institute of Health and Welfare. AIHW National Hospital Morbidity database. 2021. https://www.aihw.gov.au/reports/hospitals/principal-diagnosis-data-cubes/contents/about
3. Australian Institute of Health and Welfare. Heart, stroke and vascular disease: Australian facts. 2023. https://www.aihw.gov.au/reports/heart-stroke-vascular-disease/hsvd-facts/contents/risk-factors/multiple-risk-factors
4. Chew DP, Scott IA, Cullen L, et al. National Heart Foundation of Australia & Cardiac Society of Australia and New Zealand: Australian Clinical Guidelines for the Management of Acute Coronary Syndromes 2016. Heart Lung Circ. Sep 2016;25(9):895-951. doi:10.1016/j.hlc.2016.06.789
You might also be interested in...

Support after a heart attack
Many different thoughts may go through your head after a heart attack and you may be presented with complicated medical info. Know where to get support.

What is cardiac rehab?
Cardiac rehab is proven to keep you out of hospital and reduce your risk of death from heart conditions.
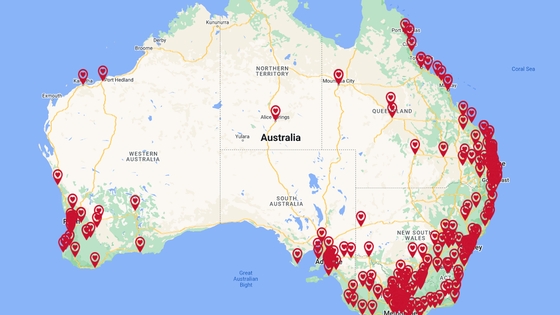
Find a cardiac rehabilitation service near you
Cardiac rehabilitation helps your recovery after a heart procedure or the diagnosis of a heart condition. It also helps lower your chances of having heart problems in the future.
Last updated08 February 2024