Heart procedures and devices
Explore heart treatments: procedures, surgeries, and devices explained
If you have a heart condition, your doctor may recommend different treatments, including procedures or devices.
Read about the different types of devices or procedures (including surgeries) that your doctor may recommend.
Ablation
An ablation (or ‘catheter ablation’) can treat abnormal heart rhythms. This procedure disrupts or deactivates the area of the heart where the abnormal electrical signals are coming from.
What does ablation involve?
- You will be given a local anaesthetic and sedation to keep you comfortable during the procedure.
- Your doctor will insert a long, thin tube (catheter) into a blood vessel in your groin (or sometimes your neck or shoulder area). The catheter has an electrode at the tip.
- The catheter is threaded up through the blood vessel until it reaches your heart.
- The electrode uses heat (radiofrequency waves) or freezing (cryoablation) to deactivate the part of the heart that’s creating or passing the abnormal electrical signals.
Ablation doesn’t usually fix the abnormal heart rhythm right away. It may take a few weeks to see if the treatment has worked or not.
Cardiac resynchronisation therapy
Cardiac resynchronisation therapy is used to help some people with a type of heart failure that involves parts of the heart contracting too early or late. This leads to less blood being pumped around your body. It uses a small device which is a special type of pacemaker, sometimes also called a ‘biventricular pacemaker’ or ‘CRT’.
The device sits under the skin on your chest, usually below your collar bone (clavicle). It has wires that connect to your heart’s chambers that produce small electrical currents to stimulate your heart to pump. This device helps the left and right sides of the heart work together. It can improve heart failure symptoms and can keep people out of hospital.
This type of pacemaker is often combined with an implantable cardioverter defibrillator (CRT-D).
Cardioversion
Cardioversion aims to return an abnormal heart rhythm to a normal rhythm.
There are two main types of cardioversion.
- Electrical cardioversion
- You will be given a general anaesthetic to put you to sleep.
- Pads are attached to your chest. The pads are connected to a machine called a defibrillator (see ‘defibrillation’).
- The defibrillator gives your heart a small electrical ‘shock’ to get the heart back into a normal rhythm. You might need more than one shock.
- Your heart rhythm will be monitored during and after the procedure, to make sure it has been successful.
Pharmacological cardioversion (cardioversion using medicines)
Your doctor will give you special heart medicines to return your heart to a normal rhythm. This is usually done in hospital so your doctor can monitor your heart rhythm to see if the medicine has worked.
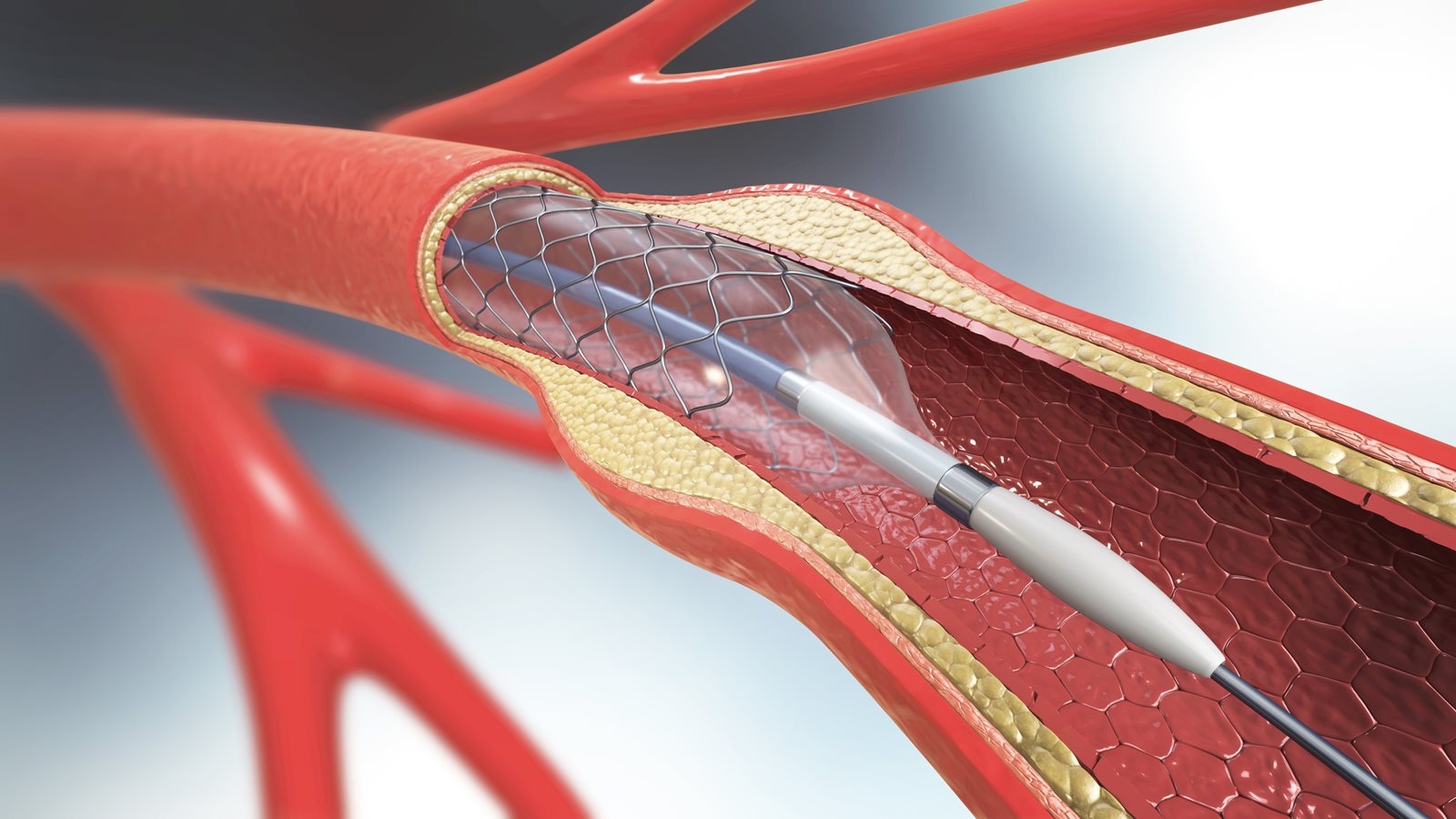
Coronary angioplasty and stent insertion
Coronary angioplasty (with or without stent insertion) is a common treatment for people with coronary heart disease, after a heart attack or angina (chest pain) episode episode (also called acute coronary syndromes (ACS)).
This procedure improves blood flow to the heart by opening the coronary arteries using a small, inflated balloon. Sometimes a stent is inserted at the same time to stop a blockage from happening again. This procedure is also called ‘percutaneous coronary intervention’.
What does coronary angioplasty involve?
- You will be given a local anaesthetic and you will be awake during the procedure.
- Your doctor will insert a long, thin tube (catheter) into a blood vessel in your groin or wrist.
- The catheter, which has a tiny balloon at the end, is threaded through the blood vessel until it reaches your heart.
- When the catheter reaches the blocked or narrowed part of your coronary artery, the balloon is gently inflated to open up the artery.
As part of the angioplasty procedure, your doctor may decide to insert a stent into the coronary artery to make sure it stays open. The stent is a small mesh tube that helps to keep your vessel open. In this case, the balloon is deflated and taken out while the stent stays in place.
Defibrillation
Defibrillation is an emergency treatment to help the heart start beating. It is used when a person’s heart has stopped beating (a cardiac arrest). It uses paddles or pads that are put on your chest to deliver a small electrical current or ‘shock’ to your heart to make it start beating regularly again.
Automated external defibrillators (AEDs) are a portable version that are kept in public places like shopping centres or sports centres. The device can be used by anyone, the unit will talk you through how to use it – no training is required!
Defibrillation can also be used to treat abnormal heart rhythms (for example, if your heart beats too fast or in an irregular way). In these non-emergency situations, you will be given a general anaesthetic, and the procedure will happen in a hospital or clinic. See ‘cardioversion’.
Depending on the heart condition you have, your doctor may recommend that you have an implantable cardioverter defibrillator (ICD) inserted. See ‘implantable cardioverter defibrillator’.
Extracorporeal membrane oxygenation (ECMO)
Some people with severe heart conditions may need the support of a special type of life-support machine (extracorporeal membrane oxygenation machine).
The machine replaces the normal action of the heart and lungs. ECMO is used when your heart and lungs need help to heal.
ECMO can be used to treat people with severe inflammation of the heart muscle (myocarditis) or those waiting for or recovering from a heart transplant. See 'heart transplant surgery'.
Heart bypass surgery/coronary artery bypass graft surgery (CABGS or CAGS)
If your coronary arteries are very narrowed or blocked, treatments like medicines, angioplasty and stents may not be effective. Your doctor may recommend heart bypass surgery depending on the location of the blockage, and how many coronary arteries are affected.
This surgery can improve blood flow to your heart, relieve angina (chest pain) symptoms and prevent future heart attacks.
What does heart bypass surgery involve?
- This is a type of open-heart surgery. You’ll be given a general anaesthetic and will be asleep during the surgery.
- Your surgeon will take a healthy blood vessel from somewhere else in your body (the chest, leg or arm).
- They will attach the healthy blood vessel above and below the blocked part of the artery. This allows blood to go around (bypass) the blockage.
Heart transplant surgery
A heart transplant is surgery to replace a heart that is not working properly with a donor heart.
A transplant is most often recommended for people with severe or ‘end-stage’ heart failure. Only a very small number of heart transplants are performed each year in Australia at specialist transplant centres.
If your doctor thinks you could benefit from a heart transplant, you will be assessed to see if you can go on the transplant waiting list. You may be added to the list right away, or your condition might not be severe enough to be added to the list. In this case, your condition will be monitored regularly, and you will be added to the list at the appropriate time.
For some people, a heart transplant isn’t suitable.
Heart valve surgery
Heart valve diseases can be treated by either manually opening up a heart valve, or fixing or replacing it.
Balloon valvuloplasty/valvotomy
This procedure is similar to a coronary angioplasty. A balloon is inserted into the narrowed heart valve using a catheter. The balloon is then inflated to widen the opening of the valve, so blood can flow through the heart more easily. If this procedure is not suitable, surgery may be needed.
Heart valve surgery
Heart valve surgery repairs or replaces heart valves that aren’t working properly and helps your heart to pump blood.
To replace the damaged valves, your surgeon will use a mechanical valve or biological tissue valve. Biological tissue valves come from pigs, cows or sometimes from human donors.
There is another type of valve surgery used to treat a condition called aortic stenosis (narrowing and stiffening of the aortic valve). This surgery is called transcatheter aortic valve implantation (TAVI), where a new valve is inserted to sit inside the damaged valve.
Read more about treatments for heart valve diseases.
Implantable cardioverter defibrillator (ICD)
An ICD is a small battery-powered box (smaller than a matchbox) that is inserted under the skin, usually in the space just below the collar bone (clavicle). Thin wires connect the ICD to the heart. The ICD continuously monitors your heart and can correct dangerous abnormal heart rhythms if needed.
An ICD can:
- correct an abnormal heart rhythm by making your heart beat regularly
- give your heart small electrical ‘shocks’ to make your beat normally again if the abnormal heart rhythm is life-threatening
- support the heartbeat (like a pacemaker) if it’s beating very slowly.
There are different types of ICDs available. Your doctor will discuss with you which ICD is most suitable for you.
ICDs can also store information about your heart's activity for your doctor to check.
Intra-aortic balloon pump
An intra-aortic balloon pump (IABP) is used when your heart isn’t pumping enough blood, or isn’t pumping effectively, such as during heart failure.
Placing an IABP is similar to a coronary angioplasty. A catheter is inserted into a blood vessel, usually in your leg/groin. The balloon is fed through the catheter until it reaches your aorta (the large vessel that takes blood from your heart to the rest of your body). The balloon inflates when your heart is relaxed and deflates when your heart contracts. This helps your heart to pump enough blood around your body.
The IABP is often only left in for a few days while you recover from a heart event, usually while you are still in hospital.
Pacemaker
The heart has a natural pacemaker to make it beat normally. The natural pacemaker (also known as the sinoatrial node) is a group of cells located at the top of the heart. The sinoatrial node sends electrical signals to the heart to make it contract and pump blood around the body. If that’s not working reliably, an artificial pacemaker can be inserted to do the same job.
A pacemaker is a small device that is put under the skin on your chest, usually below your collar bone (clavicle). It has one or more wires that connect to your heart’s chambers. A pacemaker produces small electrical currents that stimulate your heart to pump regularly.
Modern pacemakers are very comfortable and reliable. They shouldn’t affect your day-to-day life. You may need to make a few small changes for a short time. People who have pacemakers and devices need to have regular follow-up appointments to make sure the device is working well. A pacemaker battery usually lasts between five to 15 years, depending on the type of device. Your doctor will check the battery. When the battery is running low, you will need to go back to the hospital to have a new pacemaker inserted.
Percutaneous coronary intervention
Percutaneous coronary intervention (PCI) is the name for a type of coronary angioplasty used to treat narrowed or blocked vessels (see Coronary angioplasty and stent insertion above).
Thrombolysis (thrombolytic therapy)
Thrombolysis or ‘thrombolytic therapy’ is a treatment to dissolve blood clots. It is often used in people who have had a heart attack, to dissolve a blood clot that is narrowing or blocking a coronary artery. The ‘clot-busting’ medicine is given to you through a drip. Dissolving the clot improves blood flow to your heart muscle and around your body.
Ventricular assist devices
For people on the heart transplant waiting list, a type of device called a ventricular assist device can help people to survive longer. Your doctor may also recommend a ventricular assist device if you aren’t suitable for a heart transplant.
A ventricular assist device is a type of artificial heart pump that can help people with heart failure. The device is inserted into the heart to help the heart pump blood around the body more efficiently. It’s connected to a control unit that the person must wear on the outside of their body all the time.
References
- Brieger D, Cullen L, Briffa T, et al. National Heart Foundation of Australia & Cardiac Society of Australia and New Zealand: Australian clinical guideline for diagnosing and managing acute coronary syndromes 2024. Heart, Lung & Circulation. In press.
- National Heart, Lung and Blood Institute. Heart treatments. 24 March 2022. Accessed 14 January 2025. www.nhlbi.nih.gov/health/heart-treatments-procedures
- Murphy C, Zafar H, Sharif F. An updated review of cardiac devices in heart failure. Ir J Med Sci.2017;186:909–919.
- Franz T, ed. Cardiovascular and cardiac therapeutic devices. Springer; 2014.
You might also be interested in...

What is cardiac rehab?
Cardiac rehab is proven to keep you out of hospital and reduce your risk of death from heart conditions.

Understanding your heart medicines
Find out about common heart medicines

Heart medicines – Frequently asked questions
Find answers below to frequently asked questions about heart medicines.
Last updated14 October 2025
Last reviewed29 April 2025
